Socrates contemplating, By Anastasios71 on Shutterstock
COVID-19 and emotional stress trigger inflammatory immune responses. And then our brain changes. It does matter what we think and how we process events in our life.
What has your month been like? Were you able to focus on something important to you or do something fun and energizing? Did you accomplish what you intended to this month? My May 1 calendar note read, “Make sense of chaos.” I don’t remember what was going on astrologically to trigger this directive, but this was the month’s message for me. I set out with intention.
A year ago in May, we lived in a peak of uncertainty with rising COVID-19 cases and hospitalizations and intense fear of getting severely ill or dying. The pandemic still is very present around the world. Still, the acute adrenaline surge has abated for most of us in the United States, some European countries, and many islands that can keep the virus contained. Unfortunately, the effects of living through a pandemic—whether we get sick with COVID-19 or not—will be long-lasting. That’s what I learned this past week in my selective deep dive into the current state of the science and psychology of COVID-19.
When I was in academe, May typically was “conference month” for me—a month of travel and speaking and connecting and sharing and learning. This year, thanks to COVID-19 and Zoom, I had access to many annual conferences and programs (including international ones) without leaving home—saving time, energy, and money. Before I knew it, I had signed up for seven all-day or multi-day conferences and seven additional webinars or sessions. It was a bit overwhelming when some overlapped. Still, it was fun and challenging to be immersed, once again, in the science, practice, and understanding of how our minds and hearts coalesce and communicate with the cells of our bodies.
Although not all sessions were COVID specific, my goal was to translate some of the most relevant laboratory and clinical studies and insights into some coherent takeaways relevant to all of us living through a pandemic. Experts in psychoneuroimmunology reported recent studies of the brain, central nervous system, and immune responses to stress and SARS-CoV-2. Functional Medicine practitioners advised on cardiovascular, pulmonary, and neurological assessments and treatments, and others offered strategies in mind and health to improve well-being when faced with stress. COVID-19 is a complex illness requiring a multi-prong, individualized approach to understanding, assessment, and treatment. And living through a pandemic requires adaptability and flexibility.
As Scott Turow said in his author session with the Kauai Writers Conference last week, “Write what you know and are obsessed with.” However, this isn’t the intriguing courtroom, and I realize not everyone is interested in the individual study results and mechanisms of how pathology happens, so I include just the main takeaways here. If you want more detail or references, add a note in the comments.
Why COVID-19 Affects Everyone
In contrast to other respiratory illnesses, such as influenza and cold viruses, SARS-CoV-2 causes a long and variable list of potential symptoms that aren’t consistent among those getting sick. Some people get acute gastrointestinal symptoms, while others get no GI effects. Some get pneumonia or blood clots, or cardiac arrhythmias, while others get loss of taste or smell, body aches, headaches, overwhelming fatigue, or bizarre hallucinations. The list goes on, with 50 clinical sequelae identified in one retrospective study of more than 266,000 people diagnosed with COVID-19. Any combination of symptoms and severity is possible—from no symptoms or mild illness to death. Getting sick with COVID-19 can be life-threatening. And scary.
Why are some people more vulnerable to severe illness while others sneak through with minor symptoms? And what about those of us who haven’t gotten sick but have friends or family who have died? Although not as acutely stressful as gasping for air, collapsing from weakness or arrhythmias, and fearing death—your death—the uncertainty, unpredictability, and perceived vulnerability of living through the pandemic is stressful. You already knew that. Toss in loneliness from isolation (which rose 400 percent in 2020) and the risk of depression and stress skyrocket.
Stress and depression affect the immune system, making us more vulnerable to illness and COVID-19 itself. And when our immune system is weak and/or the pathogen very strong (i.e., SARS-CoV-2), we are more likely to get sick. Chronic stress is even more immunosuppressive than acute stress. (Acute stress activates immune responses and then goes back to normal through a feedback loop if the stressor abates). The longer the pandemic and our perceived stress of living through it drag on, the greater the effects on our bodies. No one on our earth is immune to COVID-19 related stress.
Coronavirus attacking human cell, By Giovanni Cancemi on Shutterstock
How Do COVID-19 and Stress Affect the Immune System?
Inflammation is key. Whether from COVID-19 itself or pandemic-related social-economic-emotional-relational-situational issues, the physical, mental, and emotional toll triggers an inflammatory response.
COVID-19
For those who have COVID-19, the immune system responds to SARS-CoV-2 (the virus) as an invader, triggering the release of pro-inflammatory cytokines (e.g., IL-6, IL-1ß, TNFα) from T, B, and natural killer (NK) white blood cells. The cytokines are the signals for the immune cells to work together to identify, engulf, and kill the invader. While it is initially protective, the immune system sometimes over-reacts and makes antibodies against itself or doesn’t shut off (there are anti-inflammatory cytokines too), causing tissue and organ destruction (blood vessels, lungs, gut, joints, kidneys, liver, pancreas, neurons). The resulting inflammation and vascular clotting explain the lung pathology, organ failure, and stroke in those who die from COVID-19. Continued secretion of pro-inflammatory cytokines has been associated with anxiety, depression, and fatigue of “Long-haulers”—those who continue to have symptoms more than a month after getting COVID-19.
Stress
Emotional stress also triggers inflammation, but our own brain activates the signal instead of an outside trigger. When we perceive a situation as stressful, the amygdala (which interprets fear and sadness and strong emotions) signals the hypothalamus, pituitary, and then the adrenal glands to secrete adrenaline (fight or flight hormone), noradrenaline, and cortisol (the hormone that gets you out of bed is also the “stress hormone”). The same white blood cells involved in inflammation have receptors for cortisol and respond by releasing inflammatory cytokines.
Inflammation follows, although with less intensity or a shorter time than with COVID, allowing for the anti-inflammatory cytokines and shut-off feedback loops to work (in most cases, but not all, which partly explains the diverse human responses). If we manage our stress (or our immune system is able to contain and kill the virus), then the inflammatory response abates, and we feel better emotionally and physically.
While acute stress upregulates the immune system (and protects us), chronic stress (over months) suppresses it. Like Goldilocks, our bodies try to find just the right balance between too much and too little activation and suppression. If our stress continues or COVID symptoms drag on into “long-haul COVID,” the inflammation continues to damage our bodies (even telomeres shorten, leaving our chromosomes more vulnerable to mutations and death) and our minds.
And…while stress triggers inflammation and immune dysregulation, the reverse pathway is also true—inflammation triggers emotional states (commonly, anxiety and depression). The bottom line is that our mental, emotional, and immune systems are intricately intertwined and communicate with each other. The greater the emotional distress, the greater the immune dysregulation, and the higher the inflammatory response, the higher the chance of emotional and mental distress.
Brain neural network, by MattLPhotography on Shutterstock
Effects on the Brain
COVID-19
Not everyone with COVID-19 gets neurological symptoms, possibly because the blood-brain barrier stops the virus from invading neurons and inflammatory cytokines from reaching targets. However, there is evidence for a direct viral invasion of blood vessel walls and neurons (both have ACE2 receptors) and indirect inflammation-causing autoimmunity. Although thrombosis/clotting in the brain could explain neuropsychological symptoms, the loss of taste and smell, dizziness, seizures, inflammation of the meninges, and loss of myelin is likely a result of cytokine release and inflammatory damage.
High levels of pro-inflammatory cytokines also have been associated with lingering anxiety, depression, and psychosis in survivors, which occur in one-third to one-half of survivors. Because symptoms are reduced when patients are given cytokine blocking agents (Anakinra or Tocilizumab, which block IL-1 or IL-6, respectively), cytokines play a clear role in mental and emotional states.
But inflammation doesn’t explain everything. Neurons in the brain can be damaged directly by the SARS-CoV-2 virus, which attaches to the ACE2 receptors. (If you block the receptors, the damage to neurons is mitigated). Swollen astrocytes and axon damage also suggest direct invasion of the virus into the brain and spinal cord. But because actual SARS-CoV-2 RNA was not found in the brains and cerebrospinal fluid of many patients, it is more likely that inflammation triggers the neurological effects of COVID-19.
Stress
Stress and depression also change the brain’s structure and can be explained in part by excess cortisol and inflammation. Some of the biological effects include:
- Atrophy (shrinking) of the hippocampus (affecting memory)
- Atrophy of the prefrontal cortex (affecting impulse control and appraisal/interpretation of events)
- Dendrites shorten in the hippocampus and prefrontal cortex (increasing processing time)
- Anterior cingulate cortex signaling changes
- Changes white and gray matter balance of the brain (affecting learning and memory)
- Neurons lose their plasticity (ability to adapt in response to challenges)
- Genes lose their regulation to turn on and off in response to environmental cues
- Neurotransmitters decrease (serotonin, dopamine, norepinephrine, BDNF-brain-derived neurotrophic factor) or increase (glutamate, substance P), resulting in rumination, mood changes, lethargy, depression, anxiety, and pain.
Our brains change structurally in response to stress, anxiety, depression, and negative self-talk, such as feeling “less than” or shame and doubt. Our thoughts really do affect our biology. But the reverse is also true—changes in brain structure cause emotional and cognitive effects. This is especially evident in people who have had strokes or brain injury. The brain has a “plasticity” in its ability to rewire itself and adapt neural circuits around the injury, which can be encouraged through practice/repetition of new ways of doing and thinking about things. We can similarly modify our habits of thought.
It does matter what we think and how we process events in our life. However, not all biological responses are under our conscious control, and we can’t reverse disease just by thinking it will get better. But here is what we can do to support our immune systems and respond to the stress of living through a pandemic.

What Can We Do?
First, it’s important to remember that our response to stress, not the stressor itself, determines how our body reacts. Focus on what you can change.
The only way to control the SARS-CoV-2 virus is to stop it in its tracks through vaccination (and prevent access to its targets by distancing and wearing masks). The more people with immunity, the fewer its targets, and it will eventually die (or at least become less prominent and virulent over time).
Meanwhile, we can manage our own stress to support our immune system’s ability to recognize and kill the virus before it causes illness and to enhance the vaccine’s effectiveness to prevent breakthrough illness. Obviously, underlying illness/conditions, genetics, and environment also influence how our bodies respond to SARS-CoV-2 and stress. But lifestyle, relationships, mindset, and our emotional stress response are things we can change to support the resilience of our immune system and brain.
Health is not a dichotomy; you are not sick or well. Our well-being encompasses body, mind, and spirit and lies on a continuum with health/wellness on one end and illness/disease on the other. Stress swings the pendulum toward illness. Managing our stress response is key to staying well.
There’s always room to improve, and well-being is a skill we all can learn through awareness, connection, insight, and purpose, according to Dr. Richard Davidson, psychologist and neuroscientist at the University of Wisconsin, Madison, who studies brain responses to meditation in Buddhist monks.
Things we can do:
- Manage Stress: mindfulness, meditation, exercise, nature, whatever works for you!
- Support the immune system: exercise (increases BDNF, other neurotransmitters), diet (more antioxidants, less sugar, which triggers inflammation), adequate sleep
- Perception check-in: find meaning, have a purpose/direction/plan, determine priorities and values (and live by them), practice gratitude
- Alter mindset: help others, be curious instead of judgmental, reframe negative thoughts.
- Stay connected: positive and supportive relationships
- Do something fun just for the joy of it
Key goals are to manage our response to stressors to be less reactive, support our immune system, and live according to our values and priorities. The stress of living through a pandemic will be long-lasting for all of us. What new and healthy strategies can you take going forward?
There is still so much to learn about COVID-19 and our physical, mental, and psychological responses to its presence in our world and our bodies (as illness, vaccine response, and stress consequences). While we continue to learn and adapt, let’s do the best we can to stay resilient and well—in body, mind, and spirit.
The best of health to you.
~ Janice
About the Book
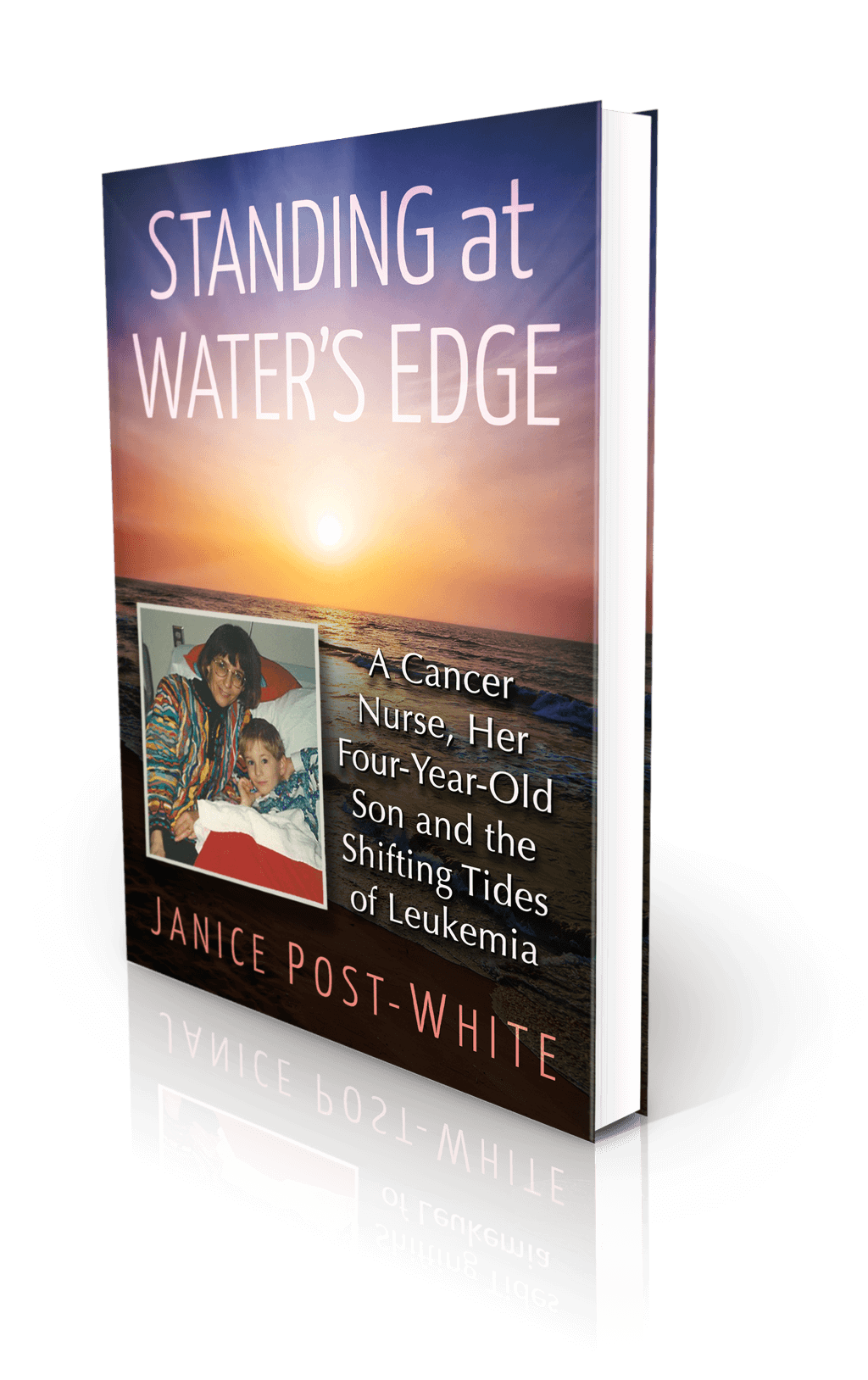
Janice Post-White’s memoir is a story about a cancer nurse who thought she knew what life and death were about.
Then her 4-year-old son got leukemia.
This heart-wrenchingly real but inspiring book shines a light on the life-affirming discoveries that can be made when one is forced to face death—and bravely chooses to face fears.
ON SALE DECEMBER 3, 2021
2022 First Place Award from the American Journal of Nursing Book of the Year in the category of Consumer Health and Third Place in Creative Works
Finalist in Health/Cancer from the American Book Fest Best Book Awards, the International Book Awards, and the Eric Hoffer Book Awards



